Understanding Antibiotic Resistance
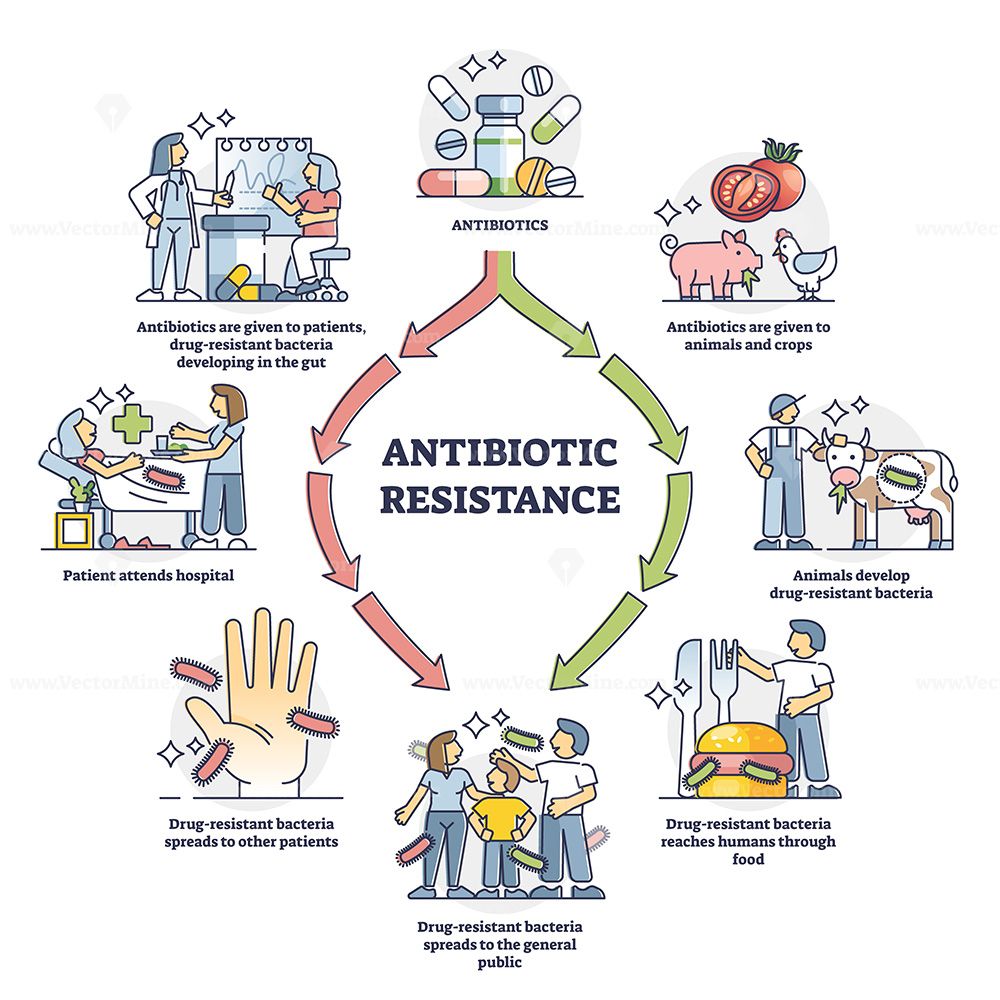
Antibiotic resistance is one of the most pressing challenges in global public health. It occurs when bacteria evolve mechanisms to withstand the drugs designed to eliminate them. This phenomenon is not a future risk — it is a present reality that threatens the efficacy of modern medicine.
Mechanisms of Resistance
Bacteria can resist antibiotics through various mechanisms, including:
- Producing enzymes that deactivate antibiotic molecules (e.g., β-lactamases)
- Altering drug targets within the bacterial cell
- Increasing efflux pump activity to expel antibiotics
- Reducing membrane permeability to prevent drug entry
Resistance genes are often carried on plasmids, enabling horizontal gene transfer between different species — accelerating the spread of resistance even across unrelated pathogens.
“Resistance is a predictable outcome of selective pressure. Misuse of antibiotics gives bacteria an evolutionary advantage.” — Dr. Irene Kapoor, Clinical Microbiologist
Impact on Modern Medicine
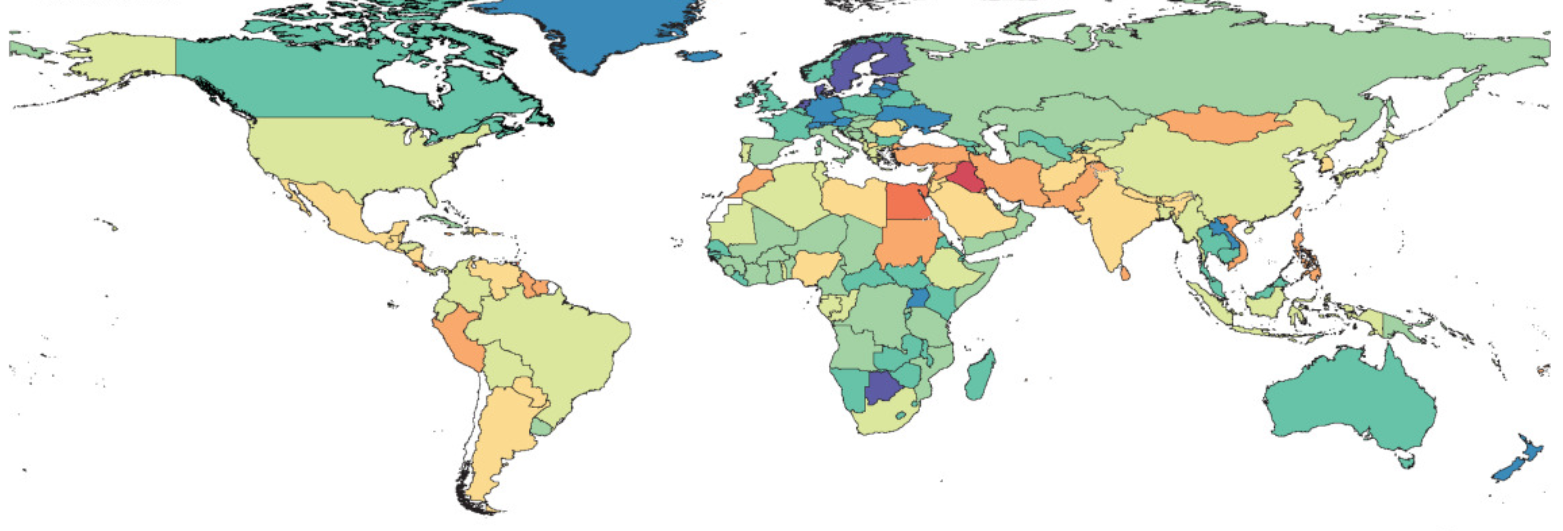
According to the WHO, over 700,000 deaths per year are currently attributable to antimicrobial resistance (AMR). If trends continue, this number could reach 10 million annually by 2050, eclipsing cancer mortality.
Common infections such as urinary tract infections, sepsis, and pneumonia are becoming harder to treat. Routine surgeries, chemotherapy, and organ transplants rely on effective antibiotics to prevent infections — resistance jeopardizes all of these.
Causes of Resistance Development
The major contributors to antibiotic resistance include:
- Overprescription and self-medication
- Non-completion of prescribed courses
- Extensive use in livestock and agriculture
- Poor infection control in healthcare settings
A 2024 meta-analysis in The Lancet Infectious Diseases found that 60% of antibiotics prescribed globally were inappropriate or unnecessary.
Antimicrobial Stewardship
In response, healthcare systems are adopting stewardship programs to ensure that antibiotics are used judiciously. These programs involve:
- Reviewing and optimizing antimicrobial prescriptions
- Educating clinicians and patients
- Promoting infection prevention through vaccination and hygiene
“Preserving antibiotic efficacy is a shared responsibility — from policymakers to prescribers to patients.” — Dr. Mahmoud El-Sayed, WHO AMR Task Force
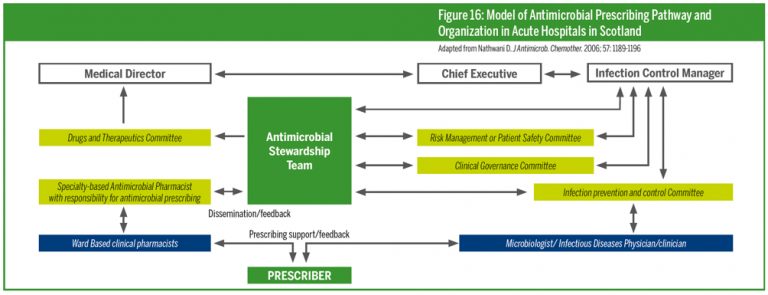
Ultimately, a multifaceted global strategy — combining policy, research, surveillance, and public education — is essential to curbing the rise of resistant infections.
← Back to Home